RESOURCES Sterility Testing

Sterility Testing
Sterility is defined as the absence of viable, contaminating microorganisms. In the pharmaceutical practice, a product is called sterile if the probability of contamination is less than one out of one million. USP requires sterile pharmaceuticals to be routinely tested for the presence of microbial contaminants. It is therefore of utmost importance to conduct sterility testing on these products. Sterility testing is a quality control test used to ensure that Compounded Sterile Preparations (CSPs) are free from microorganism contamination. With the use of proper sampling procedures, the sterility of a batch of manufactured CSPs may be properly monitored.
There are two methods in determining product sterility:
1. Membrane Filtration
Membrane Filtration is recommended for pharmaceutical products that are in filterable aqueous form, alcoholic or oily preparations and preparations miscible with aqueous or oily solvents, such that these solvents do not exhibit antimicrobial effect. Heat sensitive liquids like antibiotic solutions, toxic chemicals, radioisotopes, vaccines and carbohydrates are also suitable for membrane filtration.
USP requires membrane filter pore size to be 0.45µm or smaller to collect microorganisms effectively. Cellulose nitrate filters are commonly used for aqueous, oily and weakly alcoholic solutions; cellulose acetate filters for strongly alcoholic solutions; and specially adapted filters for specific products like antibiotics.
Membrane filtration follows the principle of physical separation of microorganisms from the filtrate. The filter containing the separated microorganisms will be segmented and transferred to appropriate sterile media. Common culture media used are Fluid Thiolglycollate Medium (FTM) and Soybean Casein Digest Medium (SCDM). The microbial content and identity can be determined after incubation.

2. Direct Inoculation
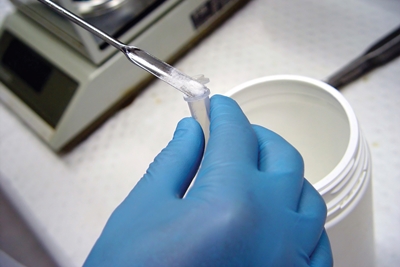
Also called Direct Transfer Sterility Testing, direct inoculation is a method used for ointments and creams, sterile devices and other pharmaceutical preparations not applicable for membrane filtration.
As the name implies, direct immersion of the sample to the media is performed in this method. Cutting the product to allow complete immersion is executed if necessary however, appropriate controls shall be strictly monitored to ensure aseptic preparation.
The volume of the product to be tested must not be more than 10% of the volume of the medium, unless otherwise prescribed. Products having antimicrobial activity must be neutralized first with a prescribed neutralizing agent or diluted with sufficient quantity of culture medium before performing the test.
FTM and SCDM culture media used in membrane filtration are also applicable for direct inoculation. Concentrated culture media may be used for large volume of samples given that subsequent dilution is possible. When needed, concentrated medium may be directly added to the product in its container. USP has set the maximum volume for media to be 2500mL. Incubation of the sample in media shall be 14 days or more.

Interpretation of Results
Microbial growth may be detected by viewing the sample against a light source. Turbid areas formed on the media may indicate microbial colonies or just a disintegrated sample which formed chemical reaction with the medium. After 14 days of incubation, transfer portions (each less than 1mL) of samples with turbid media to fresh vessels of the same medium. Incubate the original and transferred samples for not less than 4 days. Observe the culture media and determine the presence of microbial colonies.
A negative microbial growth implies sterility of the product. If microbial growth was detected, a confirmatory test shall be performed to validate the result. In the confirmatory test, the sample size used must be doubled. An investigation should also be performed to determine if the result is due to laboratory error or is inherent to the products
Variables of Sterility Testing
False positive results usually occurs due to external factors. Sterility testing requires highly trained personnel who are knowledgeable of proper sampling, preparation of media, testing procedure and constantly practice good laboratory practice. The design of the equipment and environment shall be fit in performing microbial testing. It should also be separated from other manufacturing sites and equipment to prevent contamination.
Following the pharmacopeia procedure of sterility testing does not guarantee accurate results. Validation of testing procedure and aseptic processing method is essential to be completed.